Perimenopause and fertility: Understanding your options
Perimenopause can feel like an uncertain time, especially if you’re still hoping to conceive. As hormone levels begin to shift and menstrual cycles become less predictable, you might be wondering what this means for your fertility and whether pregnancy is still possible.
While fertility naturally declines during this stage, conception can still occur. Understanding how perimenopause affects your reproductive health, and what options are available, can help you make informed choices about your next steps.
Can you get pregnant in perimenopause?
Perimenopause is the years leading up to menopause before your periods stop altogether. During this time, while your periods may become irregular, your ovaries continue to release eggs so you can still get pregnant. However, it’s less common as fertility declines with age due to several factors.
Hormones
Perimenopause is marked by fluctuating levels of key reproductive hormones, particularly oestrogen and progesterone. As these hormones become imbalanced, they can affect the regularity of ovulation, the quality of the uterine lining (needed for implantation), and overall fertility. These hormonal changes can make conceiving and maintaining a pregnancy more challenging (1).
Ovulation patterns
During perimenopause, ovulation becomes less predictable. While you may still ovulate in some cycles, others might be anovulatory (where no egg is released). The timing of ovulation can also become irregular, making it harder to track fertile windows and conceive (2).
Egg quality
As women age, the number of eggs in the ovaries decreases, but egg quality also plays a crucial role in fertility. By perimenopause, a higher percentage of eggs may have chromosomal abnormalities, which can make conception more difficult (3).
Learn more about perimenopausal changes.
Perimenopause fertility rates
Perimenopause doesn’t occur at the same time for everyone and how long it lasts also differs between individuals. However, it usually begins in a woman’s mid to late 40’s (4). Therefore, when discussing fertility rates in perimenopause, it can be helpful to look at them in comparison to fertility rates at other ages.
The chance of conception within one year is:
- 75% at age 30
- 66% at age 35
- 44% at age 40 (5)
Trying to conceive during perimenopause
While fertility naturally declines during perimenopause, pregnancy is still possible for many women. In 2021 in England and Wales, more than 28,000 women aged 40 to 44 and over 2,000 women aged 45 and over gave birth (6).
Some conceive naturally, while others may require medical assistance. Understanding the available options can help you navigate this stage with confidence and make informed decisions about the best path for you.
Natural conception
Although ovulation becomes less predictable in perimenopause, some women can still conceive naturally.
Tracking ovulation to identify your most fertile days can be useful. This can be done through:
- Basal body temperature (BBT) charting
- Ovulation predictor kits (OPKs)
- Fertility tracking apps
- Monitoring vaginal mucus (7)
Maintaining a healthy lifestyle can also support reproductive health. Steps you can take include:
- Adopting a balanced diet
- Undertaking regular exercise
- Managing stress
- Reducing alcohol intake
- Stopping smoking
- Maintaining a healthy BMI
If pregnancy doesn’t occur after six months of trying naturally, seeking specialist advice can provide further guidance.
Is it dangerous to get pregnant during perimenopause?
Many women in their 40s and early 50s successfully conceive, have uncomplicated pregnancies and deliver healthy babies but it’s important to be aware of the potential risks.
As the body transitions through perimenopause, factors like reduced egg quality, hormonal fluctuations, and underlying health conditions can increase the chances of complications including:
- Worsening of pre-existing conditions
- Gestational diabetes
- Preeclampsia
- Placental abruption
- Miscarriage
- Premature birth
- Low or high birth weight
- Genetic disorders
- Chromosomal abnormalities
- Multiples pregnancy
- Stillbirth
- Caesarean section (8,9)
Assisted reproductive technologies
For women who struggle to conceive naturally, assisted reproductive technologies (ART) can offer alternative pathways to pregnancy. Various treatments are available, depending on individual circumstances.
IUI
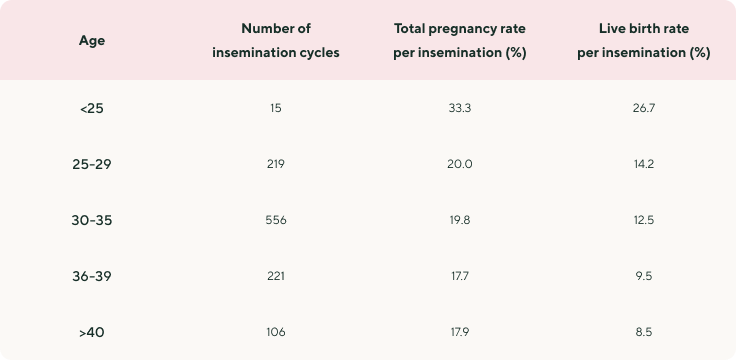
Intrauterine insemination (IUI) involves placing sperm directly into the uterus around the time of ovulation to increase the chances of fertilisation. It may be a suitable option for women who are still ovulating but experiencing irregular cycles or mild fertility challenges. However, as ovarian function declines in perimenopause, success rates may be lower than in younger women.
The results of one study (10) reveal IUI cycle outcomes by age:
IVF
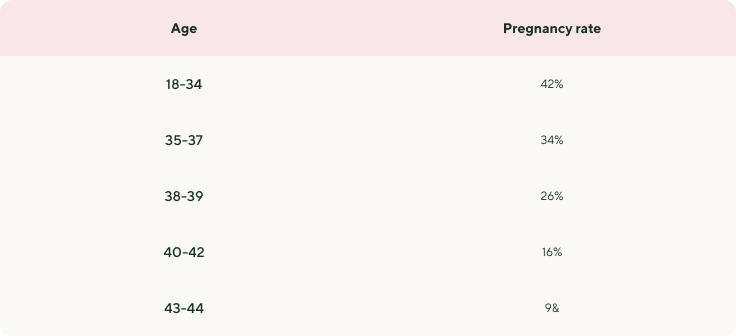
In vitro fertilisation (IVF) is a more advanced fertility treatment that involves stimulating the ovaries to produce multiple eggs, retrieving them, and fertilising them in a laboratory before transferring an embryo into the uterus. For women in perimenopause, IVF success depends largely on egg quality and ovarian reserve.
According to data from the Human Fertilisation and Embryology Authority (HFEA) (11), average fresh embryo transfer IVF pregnancy rates per embryo transferred using a woman’s egg in 2022 were as follows:
Egg donation
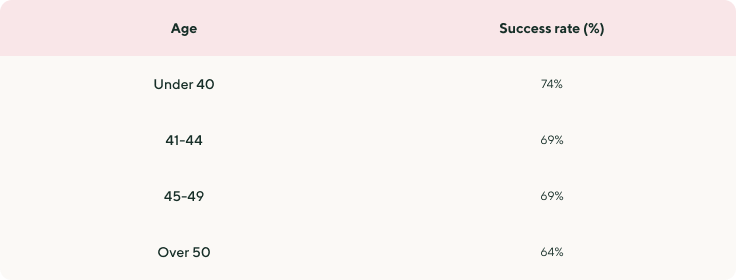
For women with diminished ovarian reserve or poor egg quality, using donor eggs from a younger, healthy donor can significantly improve the chances of conception in perimenopause. The donated egg is fertilised through IVF, and the resulting embryo is transferred into the recipient’s uterus.
A large study from the London Egg Bank (12) reveals that the overall cumulative pregnancy rate from a single cohort of donated eggs is 70% after two embryo transfers. Broken down by age range, the figures show:
Surrogacy
In cases where carrying a pregnancy may not be possible due to medical conditions or uterine issues, surrogacy offers another path to parenthood in perimenopause. This involves another person (the surrogate) carrying the pregnancy, using either the intended mother’s egg (if viable), a donor egg, or an embryo created through IVF.
Success rates for surrogacy depend on many factors, including:
- The surrogate’s ability to get pregnant
- The age of the woman whose eggs are being used
- The success of the fertility treatment (i.e., IUI, IVF or ICSI)
- The quality of the sperm used (13)
What is the maximum age for IVF on the NHS?
The National Institute for Health and Care Excellence (NICE) recommends one cycle of IVF for women under 43 who have been trying to conceive for two years, so long as they meet all other eligibility criteria. However, the upper age limit varies depending on where you live and may be as low as 35 in some areas of the UK (14).
If you are not eligible for NHS treatment, there is the option to pursue fertility treatment at a private clinic. Eligibility for and the cost of private treatment can vary significantly between clinics but can cost up to £5,000 per IVF cycle, with additional costs for tests, medications, consultation and donor eggs/sperm (14).
Planning a pregnancy during perimenopause
Careful planning can improve the chances of a healthy pregnancy during perimenopause. Understanding each stage and what support you may need can help you feel more in control of your fertility.
Preconception
Planning ahead can help improve the chances of a healthy pregnancy during perimenopause. Consulting a specialist and optimising your health before conception can make a difference.
- Consult a fertility specialist: Assess ovarian reserve, hormone levels, and general reproductive health.
- Pre-pregnancy health check: Screenings for conditions like diabetes, thyroid issues, or high blood pressure can provide a picture of your overall health.
- Track ovulation: This can help you to understand your fertile window and determine if you are ovulating each cycle.
- Consider fertility treatments: IUI, IVF, or egg donation treatment can be an option if natural conception is challenging. Your GP may be able to refer you for NHS fertility treatment or you can reach out to private clinics for further information.
- Take prenatal vitamins: Folic acid, vitamin D, and other key nutrients will help support a pregnancy (15).
Pregnancy monitoring & extra support
Pregnancies in perimenopause often require additional monitoring and support to manage potential risks. Regular health checks and specialist care can help ensure the best outcomes for both mother and baby.
- Low-dose aspirin: May be recommended to reduce the risk of preeclampsia and high blood pressure.
- Regular blood pressure checks: Help monitor for hypertension and preeclampsia risks.
- Urine monitoring: Detects protein levels, which can indicate preeclampsia.
- Growth scans: More frequent ultrasounds may be needed to track foetal development.
- Gestational diabetes screening: Higher risk due to age-related metabolic changes.
- Closer consultant-led care: High-risk pregnancies may require extra monitoring and specialist input (9).
Labour and delivery
Birth plans may need to be more flexible, as perimenopausal pregnancies carry a higher likelihood of medical interventions. Discussing options in advance can help prepare for a safe delivery.
- Early delivery discussions: Increased risk of complications may lead to planned induction or C-section.
- Induction of labour: Often recommended if pregnancy goes beyond term or complications arise (16).
- Postnatal care: Extra support for recovery, breastfeeding, and monitoring for postpartum complications.
Managing perimenopause symptoms while trying to conceive
Perimenopause symptoms, such as hot flushes, vaginal dryness, mood changes, and sleep disturbances can make the journey to pregnancy more challenging and have a profound impact on your well-being and quality of life. However, there are safe and effective ways to manage symptoms while trying to conceive.
Learn more about perimenopause and menopause symptoms.
Hormone replacement therapy (HRT)
HRT can relieve many perimenopausal symptoms. While HRT does not prevent ovulation or directly impact fertility and is not known to be harmful in pregnancy, it’s recommended that you speak with your specialist if you are planning to conceive as the decision to continue or stop HRT requires an individualised discussion. Similarly, if you become pregnant whilst taking HRT you should speak to your specialist as they may suggest altering your HRT based on your history. If you’re currently on HRT and want to consider trying to conceive, speak with your doctor about what option is appropriate for you (17).
Find out more about hormone replacement therapy.
Planning for pregnancy
If you're considering pregnancy while on HRT, it's essential to have a thorough discussion with your specialist. Together, you can assess your personal medical history and decide whether to continue, adjust, or temporarily stop HRT. This tailored approach ensures both your well-being and optimal conditions for conception.
What to do if you become pregnant
If you find yourself pregnant while taking HRT, promptly consult your specialist. They can guide you on potential adjustments to your regimen, ensuring the healthiest path forward for both you and your baby.
Lifestyle changes
Adopting healthy habits can help ease perimenopausal symptoms while also supporting fertility (18).
- Diet: A nutrient-rich diet with plenty of antioxidants, healthy fats, and protein can support hormone balance and egg quality.
- Exercise: Regular movement helps with mood, circulation, and hormone regulation but should be balanced to avoid excessive stress on the body.
- Sleep hygiene: Prioritising rest and maintaining a consistent sleep routine can improve both perimenopause symptoms and fertility.
- Stress management: Practices like yoga, meditation, or acupuncture may help regulate hormones and promote relaxation, which can reduce symptoms and contribute to better egg quality and reproductive outcomes.
With the right approach, it’s possible to manage perimenopause symptoms while supporting your fertility journey. Advice from a specialist can make all the difference. At Menopause Care, our doctors are here to help you navigate this life stage with a tailored treatment plan that addresses your concerns and aligns with your health and well-being goals. Dr Catherine Napier has specialist interests in perimenopause, pregnancy and lactation but you can also browse all menopause doctor profiles or book a free discovery call with our patient expert.
With the right approach, it’s possible to manage perimenopause symptoms while supporting your fertility journey. Advice from a specialist can make all the difference. At Menopause Care, our doctors are here to help you navigate this life stage with a tailored treatment plan that addresses your concerns and aligns with your health and well-being goals.
Dr Catherine Napier has specialist interests in perimenopause, pregnancy and lactation but you can also browse all menopause doctor profiles or book a free discovery call with our patient expert.
Perimenopausal conception - PubMed (November 2003)
What is the menopause? (August 2023)
Age and Fertility (2012)
Twice as many 40-plus women as teenagers are having babies (January 2023)
Advanced Maternal Age (Geriatric Pregnancy): Definition & Risks (February 2022)
Having a baby over the age of 40 (November 2022)
IVF - NHS (October 2021)
Vitamins, minerals and supplements in pregnancy - NHS (September 2023)
In Due Time: Pregnancy Beyond 40 and Induction of Labour (October 2017)
Planning your pregnancy - NHS (April 2023)